March 27, 2018 by Chain Drug Review
Amazon, Amazon's health care aspirations, health care, Jeff Bezos, Joseph Johnson, L.E.K. Consulting, PBM, pharmacy benefit manager, retail pharmacy, Rob Haslehurst, telemedicine
Business, Featured Articles, Leading Headlines, Pharmacy, Retail News

BOSTON — Online retail giant Amazon will enter the broader health care market — it’s just a question of how, according to global management consulting firm L.E.K. Consulting. In a new report released yesterday, L.E.K. said Amazon has the right combination of capabilities for “its big health care-industry ambitions” and could launch offerings running the gamut from
December 13, 2017 by Chain Drug Review
B. Douglas Hoey, DIR fees, Examining the Drug Supply Chain, Mark Merritt, National Community Pharmacists Association, NCPA, PBM industry, Pharmaceutical Care Management Association, pharmacy benefit manager, prescription drug costs, U.S. House of Representatives Energy & Commerce Committee, video
Videos
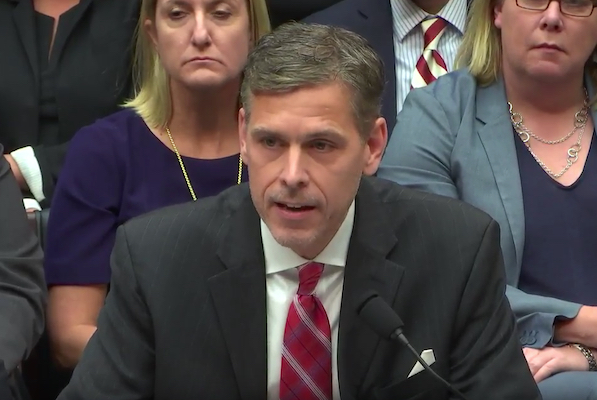
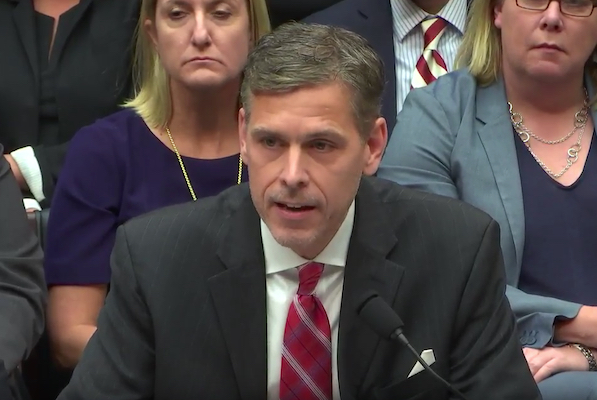
At a health subcommittee hearing of the U.S. House of Representatives Energy & Commerce Committee, B. Douglas Hoey, CEO of the National Community Pharmacists Association (NCPA), called for legislative and regulatory action on pharmacy benefit manager (PBM) business practices to help rein in prescription drug costs. The hearing, titled “Examining the Drug Supply Chain”
November 16, 2017 by Chain Drug Review
Albert Thigpen, Diplomat Pharmacy, Joel Saban, LDI Integrated Pharmacy Services, Len Dino, National Pharmacy Services, pharmacy benefit manager, Phil Hagerman, specialty pharmacy
Business, Featured Articles, Leading Headlines, Pharmacy, Retail News

FLINT, Mich. — Diplomat Pharmacy Inc. plans to acquire St. Louis-based pharmacy benefit manager LDI Integrated Pharmacy Services for in a $595 million cash and stock deal. The move marks the second PBM acquisition this month by Diplomat, the nation’s largest independent specialty pharmacy. On Nov. 6, the company announced the purchase of National Pharmacy
October 18, 2017 by Bill Schiffner
Anthem Inc., Anthem's pharmacy business, Brian Griffin, CVS Caremark, CVS Health, CVS Pharmacy, Express Scripts, IngenioRx, Larry Merlo, MinuteClinic, pharmacy benefit manager
Featured Articles, Leading Headlines, Pharmacy, Retail News

WOONSOCKET, R.I. — CVS Health has signed a five-year agreement to provide services to support IngenioRx, a new pharmacy benefit manager formed by Blue Cross Blue Shield health insurer Anthem Inc. CVS said Wednesday that its CVS Caremark PBM division will manage certain services for IngenioRx, including claims processing and prescription fulfillment. In addition, CVS
October 4, 2016 by Chain Drug Review
CVS, Deutsche Bank Securities, Express Scripts, George Hill, PBM, pharmacy benefit manager, Tricare, Walgreens
Leading Headlines, Pharmacy, Retail News
ST. LOUIS — Express Scripts Inc. is changing out CVS Pharmacy for Walgreens in its retail pharmacy network for TRICARE, the U.S. military’s health care and drug benefits program. Plans call for Walgreens pharmacies to join the Express Scripts network for TRICARE on Dec. 1. At that time, CVS pharmacies — including CVS locations in
March 17, 2016 by Chain Drug Review
Alex Gourlay, Larry Renfro, OptumRx, PBM, pharmacy benefit manager, pharmacy care, prescription drug services, Walgreens
Featured Articles, Leading Headlines, Pharmacy, Retail News

DEERFIELD, Ill. and EDEN PRAIRIE, Minn. — Walgreens and pharmacy benefit manager OptumRx are collaborating on an an integrated pharmacy care solution that blends attributes of in-store and mail-order prescription drug services. The companies said Thursday that OptumRx members enrolled in the program will get the option to fill 90-day prescriptions at home delivery co-payment levels at